Interventionalists are accustomed to extensive regulations in nearly all aspects of their field, and so are very surprised to discover that the protective quality of their lead aprons is very loosely regulated, resulting in great variation between similarly labeled products. Especially when buying a lightweight non-lead apron, they don’t know what they are getting without complicated laborious in-house testing which is usually beyond their reach. This article outlines the problems and provides some practical tips to avoid the pitfalls that lead to years of silent overexposure.
By Chet R. Rees, MD, Victor Weir, PhD., DABR, Andrew Lichliter, MD, and Evans Heithaus MD
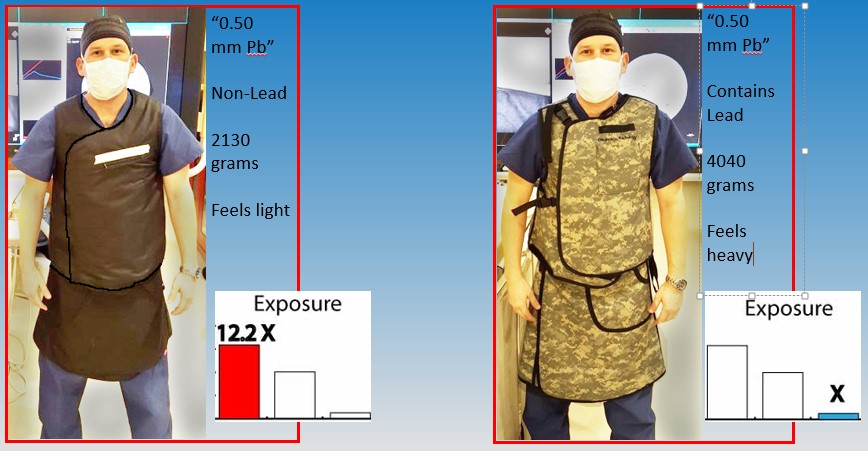
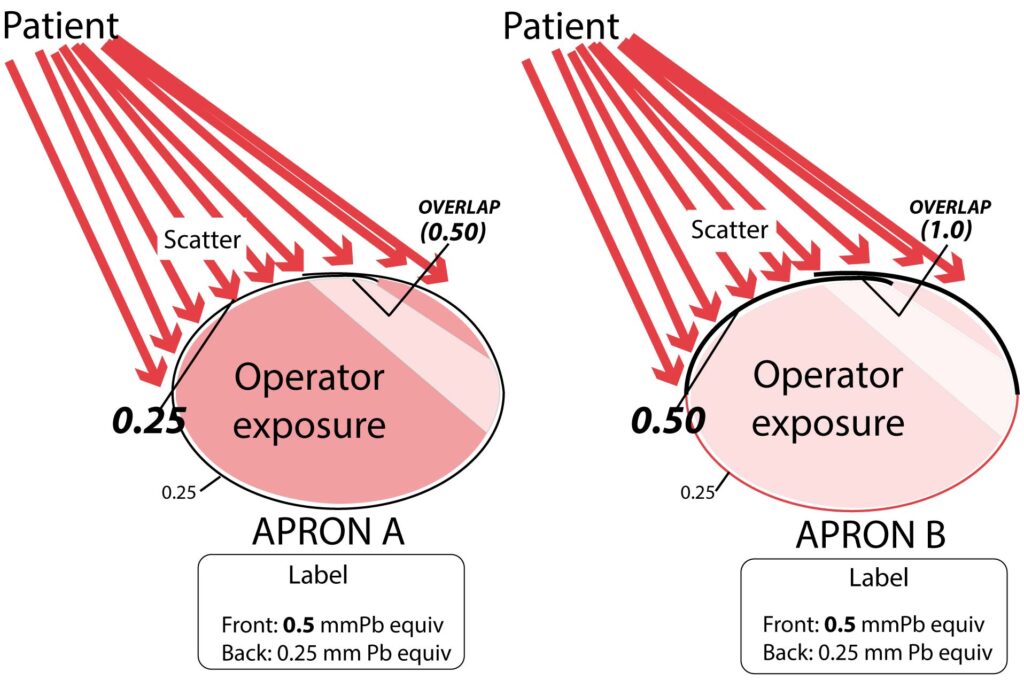
About 40-50% of interventionalists have switched to lightweight “lead” aprons (usually non-lead in reality) to deal with the musculoskeletal problems and fatigue that plague the profession and result in pain, injury, and limitation causing decreased quality of life, and reduction of case-load or disability (1,2). Most are not aware that several studies demonstrate that lightweight aprons don’t fully protect, and they may be receiving radiation exposures several times higher than if wearing standard non-lightweight aprons, despite indistinguishable labels and manufacturer-provided information. For example, one study showed that 73% of 41 aprons tested were outside tolerance levels (4), and there are many others showing the inadequacies of products, standards, and regulations in this industry (3-10). The following example may help frame the problem and its magnitude (Fig 1).
How can two aprons with the same label differ so remarkably in their protection? It is due to a combination of loose regulations, optional and outdated standards for testing, and the difference in physical properties for lead and non-lead materials which are often not accounted for in the tests. These problems include:
The radiation attenuation (blocking power) of non-lead materials is very energy dependent (fig 2) (3,5,7-9,13,14). Vendor-reported testing is frequently at only one beam quality (related to energy spectrum), while protection at other important unreported energies to which the operator is being exposed may be lower than expected by label interpretation (9). Think of two pairs of sunglasses which both appear equally dark and protective, but one doesn’t block damaging invisible UV rays, whereas the other pair does. If the labels reported only the ability to block visible light, or red light, or blue light, or any color, the user could not know which pair to buy and could receive UV damage with the first pair. Fortunately, consumers are now protected by sunglass labels which report the UV blockage values. But apron labeling is still outdated and paradoxically aprons have gotten less protective overall than the older ones (which contained lead) because the outdated standards worked well for lead, but not for the more recent non-leads which are often used in lightweight aprons.
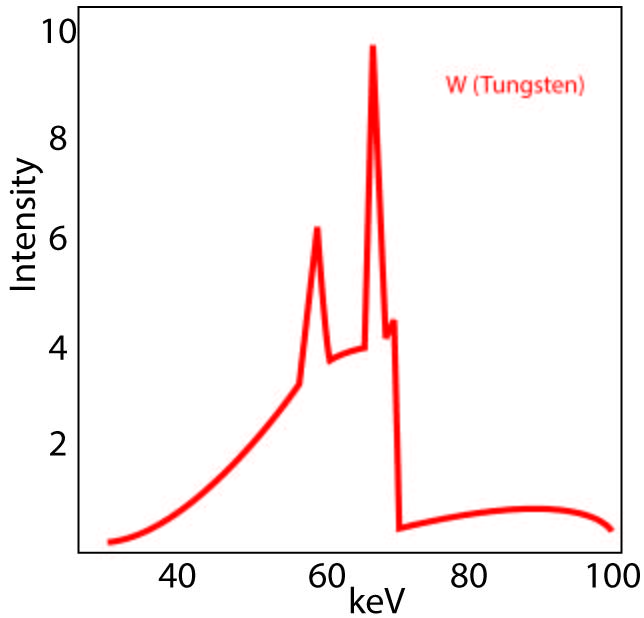
Attenuating materials, particularly non-leads of lower atomic number, actually emit secondary radiation (or fluorescence) when exposed to radiation. This new radiation reaches the operator and is of biologically damaging energies (19), however is not well detected with the most commonly used testing methods (narrow beam geometry). Use of more appropriate, but not required, testing methods (broad beam or inverse broad beam) would expose the poor protection of the lightweight aprons, despite their labels (5,8-10,13-15).
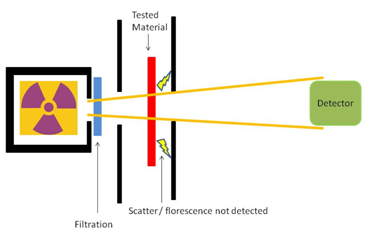
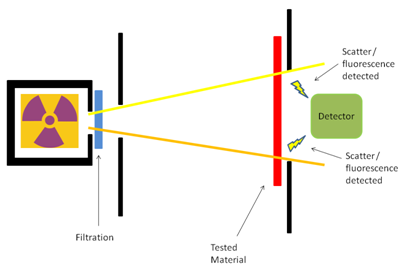
The methods recommended by standards bodies are not required, and are mostly outdated and inadequate. ASTM does not require broad beam geometry and does not provide for Pb equivalency though used on the label. The effects of somewhat improved IEC-616331-1:2014 are unknown and have yet to be realized in commercial products. Manufacturer’s labels continue to be poorly representative of protection, especially for non-leads.
The labels of some vests and skirts specify lead equivalencies that may correspond only to a double layer (overlap zone) without being clear (3). This creates confusion and may lead the user to believe the entire garment is twice its actual thickness.

Substantial weight reductions with equivalent protection have not been achieved for commercial Non-Pb garments, and protection depends largely on weight of the apron for lead and non-lead. Materials that attenuate similarly to Pb over the relevant energy range are still heavy, especially when secondary radiation is measured. Commercial claims of great weight reductions without compromise of protection are made without supporting documentation. This is more recently noted even by manufacturers, such as the statements from one company website that “…there are miniscule differences in the weights of the powders used to produce radiation protection materials…there are no secret formulas…the bottom line here is, it’s lighter weight, it is not offering the same protection levels…Plus or minus a very small percentage, a true 0.5mm [lead equivalent] LE apron is going to weight the same from one manufacturer to the next” (21). Although these facts are becoming more widely understood, under protective aprons are still on the market and need to be avoided.
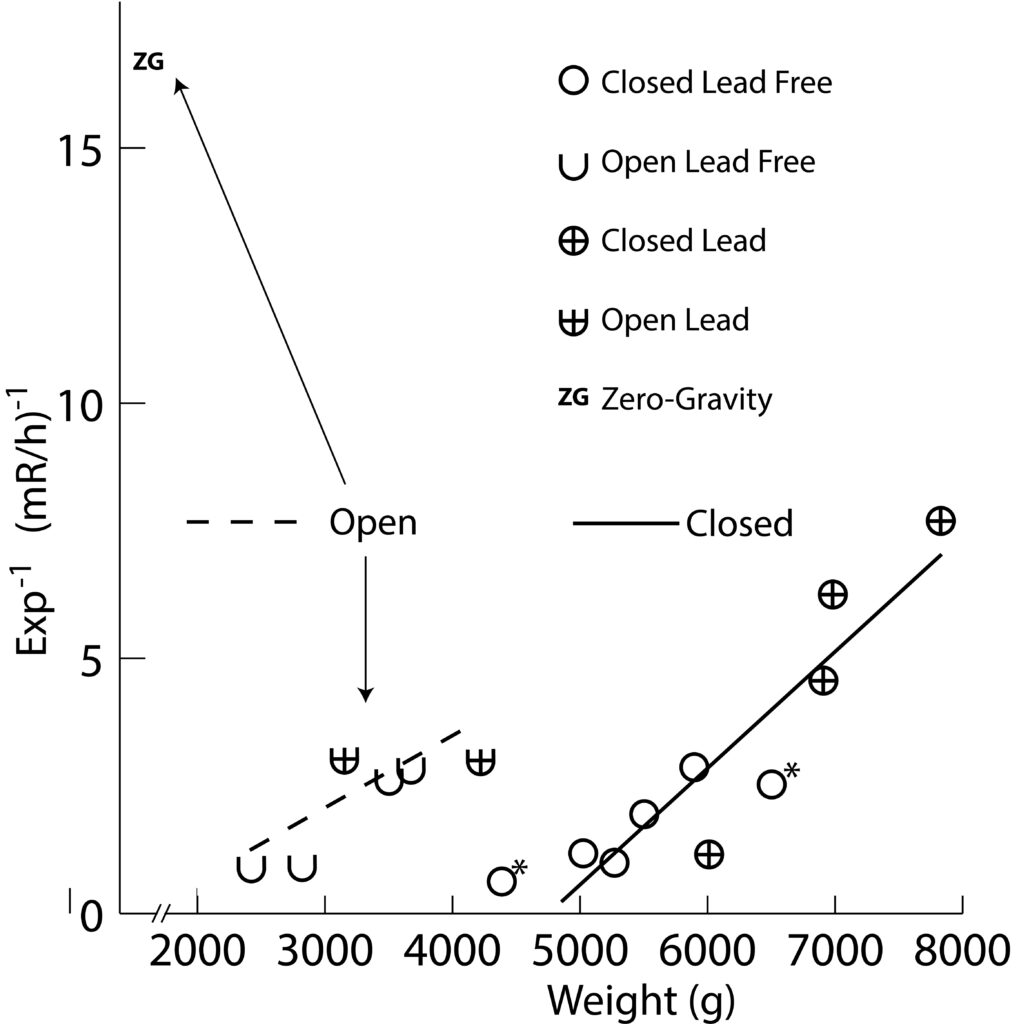
An excellent study by Pasciak, et al. (22), shows this relationship nicely in their figure 8, where 5 aprons materials were tested along with different thickness of lead foil. Lead foil offered the best protection per weight, and 4 of the 5 aprons fell on a separate line of weight vs. protection which paralleled the pure lead, owing to extra weight due to matrix and fabric. The fifth apron was an outlier; a non-lead with very poor protection per weight. Two aprons met their labels of 0.5 mm equiv (1 non-lead and 1 lead), and the other 3 failed to varying degrees, with as much as ~3X as much exposure to operator. The best protection was provided by the sole lead-based apron. In another study by Lichliter, et al (23), exposure to a phantom operator “wearing” several test aprons was measured while positioned realistically near a phantom patient creating scatter. It had several advantages over previous studies because it tested actual scattered radiation, used a clinically realistic setup, and accounted for differences in the form of the apron (such as open-back vs. closed-back, and differences in how overlap is treated as outlined in Fig 4) rather than just testing scraps of fabric. As seen in Fig 5, weight correlates very well with 1/exposure creating an almost straight line. Data fell along two lines; one for closed-back models and the other for open-back, showing that it is not necessary to cover the back when it is not turned to the patient during fluoroscopy, and that open-back designs are lighter in weight for equivalent protection since they don’t have heavy material in the back. In fact the best protection was provided by an open-back design, Zero-Gravity ™ due to it’s 1.0 mm Pb thickness. Exposures in it were 9.8% of the mean for all aprons, and 37.5% of the best apron. The most protective apron was quite heavy and worn very infrequently in the department.

HOW TO BUY AN APRON:
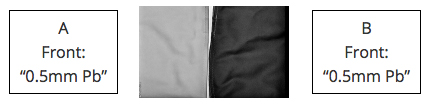
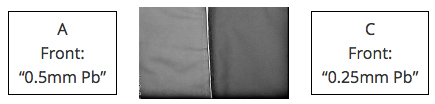
The easiest way to safely buy an apron with reasonable assurance of its protection is to buy a lead or lead-composite apron labeled 0.5 mm Pb equiv which does not feel lightweight, and if it is an overlapping design, check it with fluoroscopy to make certain it is not labeled misleadingly as shown in Figs 4-5. This is done in two ways. First, look for transition points between the back panel and the higher attenuating front panel, which if present, means the frontal Pb equivalency may not depend on overlap (e.g. Apron B in figure 5). If the apron is the same all the way around, as in Apron A of Fig 5, and the label suggests the front is twice the thickness of the back, then the apron is labeled misleadingly and it is probably best to avoid the apron and its manufacturer and vendor. Second, place the new apron side by side under fluoroscopy with an old trusty lead apron that has been tested in the past, and is labeled with the same Pb equivalency. They must be side to side due to the automatic brightness control (separate exams will not work). This test is crude and only under one beam quality but can help to distinguish large differences or misleading labeling based on overlap only.
If you need to cut a little weight, consider an open back “butcher” style apron with a good waist band to take weight off the shoulders. Get lead-based material and make sure it does not feel lightweight. Consider the fluoro test against a trusty known apron to look for gross problems.
If you insist on non-lead, insist on a label designating testing using IEC-616331-1: 2014-05 and IEC-616331-3:2014-05 (they must say 2014 in the titles) and look for the following information: Broad beam geometry (or with inverse broad beam, but NOT with narrow beam) indicated on label. Results of tests at 5 energies ranging from 30-150 kVp or wider using the beam qualities specified in Table 1 of the IEC document. The document is vague on exactly what beam qualities must be used and how to report it, so it is important to check carefully. If not on label, request source documentation which specifies the beam qualities in Table 1 of the IEC document. Unfortunately this document is copyrighted and must be purchased in their web store. It may be nearly impossible to obtain all of this information from the vendor, and as of late 2015 most manufacturers can’t provide all of it even on request (24). Ultimately, the garment should be tested in house by a physicist with a copy of the IEC-616331-1:2014 who has the set-up and knowledge to do this. This will be unavailable at most institutions. Until things change considerably with good validation in the literature, this author strongly advises against lead-free materials, especially since they do not save significant weight even when offering similar protection, and are more likely to be poorly represented by their labels.
If your back or neck is killing you and you can’t do your job without a lightweight apron, be aware that you are probably making a trade-off between weight and radiation protection. It would still be wise to test it against other options in-house using acceptable methods to make certain it is not one of the worst. Even a simple side by side fluoroscopic evaluation may be better than nothing, but the value of this has not been established.
Regulations are unlikely to change soon, and the standards are not preventing high variability of products. The only way to remedy these problems are to police the manufacturers and vendors ourselves by demanding copious technical information, making careful choices, and testing and rejecting aprons and vendors who can’t provide information or who provide misleading information.
About the author: Chet R. Rees, MD is a practicing interventional radiologist and Clinical Professor in Dallas, TX at the Baylor Scott and White Hospital. He discloses no conflict of interest in the protective apron industry. He discloses a financial interest with CFI Medical Solutions, who makes shielding products including the Zero-Gravity ™ suspended radiation protection system.
FAQ
- Q: Do substantially lightweight aprons provide adequate protection? A: No, not even when the label implies they can. There is no miracle material which dramatically cuts weight without making sacrifices in protection. The literature has shown that modest weight reductions may be achieved by mixing metals compared to using pure lead, but substantial weight reductions for same protection has been an elusive goal, despite the appearances of labels and manufacturer’s claims.
- Q: Does the “0.5 mm Pb equivalent” label on my apron mean I am protected? A: If your apron contains lead and it is not lightweight, it probably does mean you are getting the protection close to what you were expecting based on the label. But if your apron is non-lead, such labels usually do not guarantee such protection.
- Q: Is there any type of label I can trust for non-leads? A: Maybe, time will tell. The IEC-616331-1:2014 (it must say 2014 in the title) standards have incorporated some improved methods including inverse broad beam geometry and suggestion for multiple energies. However whether these are used, followed as intended, or how the results compare to independent tests are a still unknown. This author has never seen a full IEC-616331-1:2014 label on any product despite frequent checks at vendors booths.
- Q: Are all non-lead aprons terrible? A: No. Some models are not lightweight, use a good mixture of metals to provide attenuation over a spectrum of energies, and include enough to be effective. Based on reports, this seems to be the minority. Current labeling and marketing information are not very helpful, but picking them up and feeling their weight is a pretty good indicator. Unfortunately again, studies have shown that some non-lead aprons provide less protection even on a per weight basis, in addition to the loss of protection due to being lightweight, thereby being especially poor (22,23).
- Q: How do I test my apron to be sure I am okay? A: If your apron contains lead and is not lightweight, it is probably okay, but you can test at a couple beam qualities using narrow or broad beam geometry which may be available to your physicist and compare results to the attenuation tables and Pb equivalency tables, or test against a known standard. Fluoroscope any overlapping models to make sure the labeled attenuation does not correspond to overlap zone only. If your apron is non-lead, it may be difficult or impossible for you to get it done in house. Set up a broad beam geometry, and use 5 beam qualities ranging from 30-150 kVp with the beam filtration values shown in the tables in IEC-616331-1:2014. Compare results to the attenuation tables and Pb equivalency tables. Fluoroscope any overlapping models to make sure the labeled attenuation does not correspond to overlap zone only.
- This stuff scares me. How can we fix this? A: Major changes in regulations could help but will not happen anytime soon. Rapid change is possible through user awareness and demands made upon vendors. If physicians and other workers refuse to buy from vendors whose aprons haven’t been tested in rigorous ways with test values and conditions indelibly attached to the garment, then some vendors will provide the necessary information, it will be more accurate, and the quality of their aprons will have to improve since under-performing models will be exposed. Vendors who don’t do this will probably continue but at least the user will have a choice they do not have right now.
- Q: Why do manufacturers use non-leads to make lightweight aprons if non-leads aren’t really significantly more protective per weight? Why not just use thinner lead preparations? A: We can’t know the intentions, but we can state a couple things which might lead to this. First, commonly used testing such as with narrow beam geometry and use of one or two beam qualities are reasonably accurate for lead but not for non-leads; a poorly protective lightweight non-lead apron could slip through the cracks and get a 0.5 mm Pb label much more easily than a poorly protective lightweight lead apron. Second, lightweight aprons sell, they are in demand, and can command higher prices which may lead to higher profit margins. The buyer may easily believe that non-leads are lighter than lead and so can therefore make lighter aprons (when in fact aprons can easily be made to any weight using any substance in different amounts). Taken all together, the users can easily go down the intuitive, but incorrect, path that lighter materials are more efficient and make protective lightweight aprons which they should pay more money to obtain. And the sellers are simply offering what the people want, without violating any regulations or laws. The cycle can only be broken by user awareness and demands made upon vendors so that profits come to those providing good solid protection with complete and appropriate test results, not from well marketed lightweight aprons which protect worse than evident from label.
- Q: Is there any use for a lightweight apron? A: Probably yes. Some personnel don’t get very close to the patient (source of scatter radiation) during procedures, such as a circulating technologist who is usually behind the control panel. The inverse square law reduces the field in their location enough such that 0.5 mm Pb equivalency is not required. However, they should still be able to assess their purchases by label and brochure without taking wild guesses as to actual protection. For example, settling for 0.25 mm Pb equivalency but getting something less is not acceptable. Interventionalists standing near the patient should be using 0.5 mm Pb equiv without deficiencies.
- Q: Weren’t there studies that showed that non-lead bilayers could substantially lower weight without loss of attenuation? A: Two studies raised hopes of 25% weight reduction with equivalent attenuation, however these were experimental, included non-commercial metals and computer-based simulations (13,15). The authors noted that actual attenuating capabilities must be measured in the final product since it is influenced by the matrix materials and other manufacturing factors which they did not account for. Such findings in commercially available aprons have not been demonstrated to our knowledge.
REFERENCES
1. Klein, LW, Tra Y, Garratt KN, et al. Occupational health hazards of interventional cardiologists in the current decade. Catheterization and Cardiovascular Interventions 2015. 86 (5) 913-924, November 1.
2. Ross AM, Segal J, Borenstein D, Jenkins E, Cho S. Prevalence of spinal disc disease among interventional cardiologists. Am J Cardiol. 1997 Jan 1;79(1):68-70.
3. Muir S, McLeod R, Dove R. Light-weight lead aprons—light on weight, protection, or labeling accuracy? Australas Phys Eng Sci Med 2005 Jun;28(2):128-30.
4. Finnerty M, Brennan PC. Protective aprons in imaging departments: manufacturer stated lead equivalence values require validation. Eur Radiol 2005 Jul;15(7):1477-84.
5. Eder H, Panzer W, Schofer H. Is the lead-equivalent suited for rating protection properties of lead-free radiation protective clothing? Rofo 2005 Mar;177(3):399-404.
6. Vaiciunaite N, Laurikaitis M, Laurikaitiene J, Cerapaite-Trusinkiene R, Adlys G. Verification of lead equivalent for protective aprons used in radiology. Ninth International Conference & Workshop “Medical Physics in the Baltic States” 2011. Available from: http://www.medphys.lt/medphys2011/images/contributions/MedPhys2011_01_03_Vaiciunaite.pdf.
7. Eder H, Schlatt H, Hoeschen C. X-ray protective clothing: does DIN 6857-1 allow an objective comparison between lead-free and lead-composite materials? Rofo 2010 May;182(5):422-8. doi: 10.1055/s-0028-1110000.
8. Christodoulou EG, Goodsitt MM, Larson SC, Darner KL, Satti J, Chan HP. Evaluation of the transmitted exposure through lead equivalent aprons used in a radiology department, including the contribution from backscatter. Med Phys 2003 Jun;30(6):1033-8.
9. Jones AK, Wagner LK. On the futility of measuring the lead equivalence of protective garments. Med Phys 2013 Jun;40(6):063902-2:063902-9. doi: 10.1118/1.4805098.
10. Pichler T, Schopf T, Ennemoser O. Radiation protection clothing in X-ray diagnostics – comparison of attenuation equivalents in narrow beam and inverse broad-beam geometry. Rofo 2011 May;183(5):470-476. doi: 10.1055/s-0029-1245996.
11. US Food and Drug Administration [Internet]. Silver Springs (MD) [updated 2014 Sept 1; cited 2014 Sept 24]. Available from: http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/cfrsearch.cfm?fr=892.6500.
12. INFAB Corp [Internet]. [cited 2014 Sept 24]. A challenge to BLOX-R and a warning to anyone involved in the use or procurement of flexible radiation materials. Available from: http://www.infabcorp.com/open-letter-to-bloxr/.
13. McCaffrey JP, Mainegra-Hing E, Shen S. Optimizing non-PB radiation shielding materials using bilayers. Med Phys 2009 Dec;36(12):5586-5594.
14. Schlattl H, Zankl M, Eder H, Hoeschen C. Shielding properties of lead-free protective clothing and their impact on radiation doses. Med Phys 2007 Nov;34(11):4270-80.
15. McCaffrey JP, Tessier F, Shen H. Radiation shielding materials and radiation scatter effects for interventional radiology (IR) physicians. Med Phys 2012 Jul;39(7):4537-4546. doi: 10.1118/1.4730504.
16. McCaffrey JP, Shen H, Downton B, Mainegra-Hing E. Radiation attenuation by lead and nonlead materials used in radiation shielding garments. Med Phys 2007 Feb;34(2):530-537. doi: 10.1118/1.2426404.
17. ASTM International (West Conshohocken, PA). Standard test method for determining the attenuation properties in a primary X-ray beam of materials used to protect against radiation generated during the use of X-ray equipment. Designation F2547-06. Available through http://www.astm.org/Standards/F2547.htm.
18. International Electrotechnical Commission [Internet]. c2014. [cited 2014 Sept 24]. Available from: http://webstore.iec.ch/Webstore/webstore.nsf/ArtNum_PK/49622!opendocument&preview=1.
19. Schmid E, Panzer W, Schlattl H, Eder H. Emission of fluorescent x-radiation from non-lead based shielding materials of protective clothing: a radiobiological problem? J Radiol Prot 2012 Sept;32(3):129-139. doi: 10.1088/0952-4746/32/3/N129.
20. Akber SF, Das IJ, Kehwar TS. Broad beam attenuation measurements in lead in kilovoltage X-ray beams. Med Phys 2008;18:197–202. doi: 10.1016/j.zemedi.2008.04.008.
21. http://www.infabcorp.com/is-your-lead-apron-protecting-you/ Access date 2-23-2016.
22. Pasciak AS, Jones AK, Wagner LK. Application of the diagnostic radiological index of protection to protective garments. Med Phys 42 (2), February 2015. 653-662.
23. Lichliter A, Gipson S, Heithaus E, Syed A, Weir V, West J. Clinical evaluation of protective garments with respect to garment characteristics and manufacturer label information. Presentation and poster at the International Symposium on Endovascular Therapy (ISET) 2016, February 6-10, Hollywood Florida. Abstract: J Vasc Interv Radiol 2016;27:e1-e21, page e1-e2. http://www.jvir.org/article/S1051-0443%2816%2900020-8/pdf Abstract and Poster: https://www.eventscribe.com/2016/posters/ISETCIO/SplitViewer.asp?PID=MjYyNjA1MDAyNQ
24. Heithaus RE, Onofrio A, Weir V, Rees CR. Can aprons be properly evaluated for their protective quality without in-house validation? Poster at the International Symposium on Endovascular Therapy (ISET) 2016, February 6-10, Hollywood Florida. Abstract: J Vasc Interv Radiol 2016;27:e1-e21, page e11. http://www.jvir.org/article/S1051-0443%2816%2900020-8/pdf Abstract and Poster: https://www.eventscribe.com/2016/posters/ISETCIO/SplitViewer.asp?PID=MjYyNjg3MDAwOQ